If your platelet count falls under the standard concentrations during the pregnancy, you will probably have a prevalent pregnancy disorder named “gestational thrombocytopenia.”
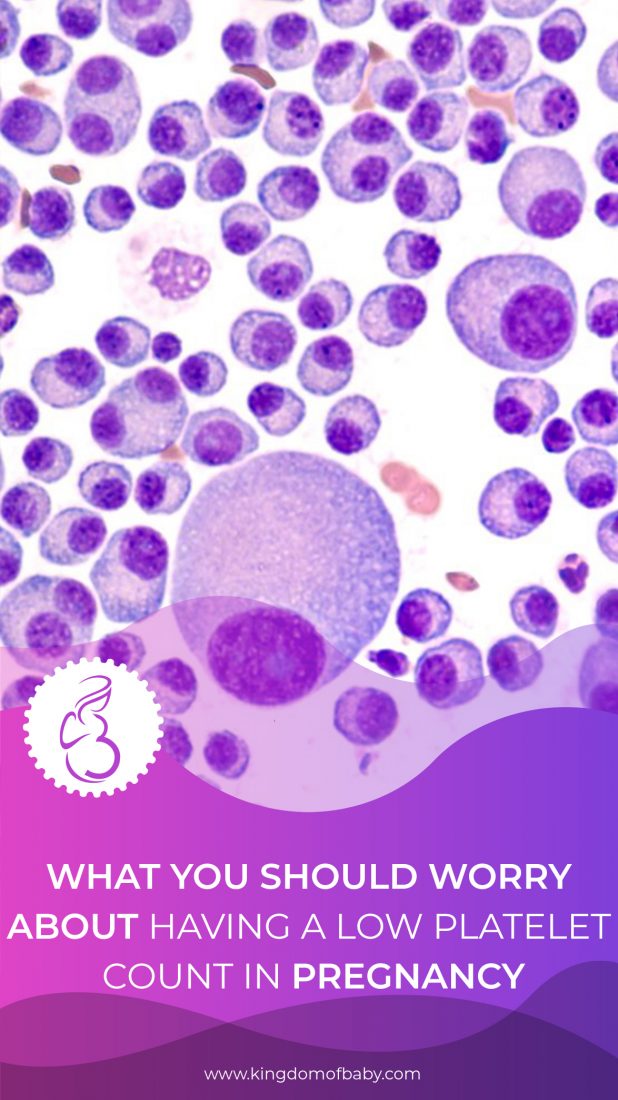
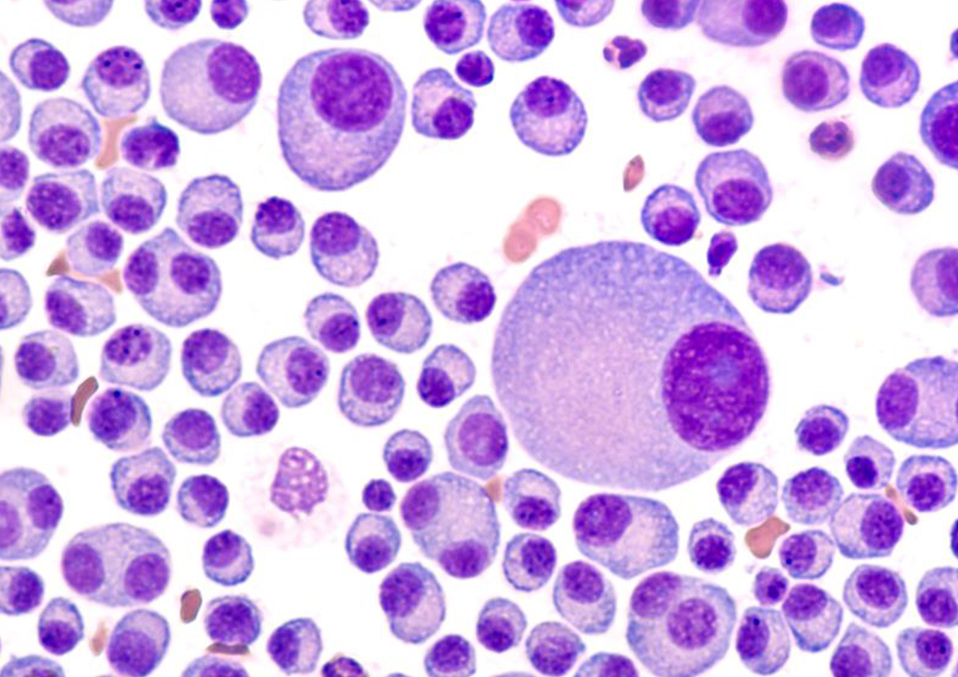
“Thrombocytopenia” is an incredibly low platelet count condition. Platelets are tiny, disc-shaped blood-clotting cells. An individual may bleed to death even from a single cut without platelets or sufficient platelets if no further treatments are applied. Normal platelet counts range from 150,000 to 400,000 platelets an ml of blood.
What are platelets?

Platelets are small cells in the blood that assist your body to develop coagulation to prevent bleeding. Send signals to the platelets when one of your blood vessels is damaged. The platelets rush to the harm site. To solve the harm, they form a plug (clot).
The process by which a damaged blood vessel is spread across the surface to prevent bleeding is called adhesion. It is because when platelets get to the damage position, they generate sticky appendages which support them to stick (adhere) to each other.
What does it mean when you have a low platelet count in pregnancy?
If your skin is wounded or broken, platelets clump and form coagulation to prevent bleeding. You can’t develop clots when you don’t have sufficient platelets in your blood.
Thrombocytopenia may also be called a low platelet count. Depending on the underlying cause, this disease can vary from mild to severe.
For some, the symptoms may include severe bleeding and, if not handled, may be deadly. There may be no symptoms for other individuals.
Thrombocytopenia during pregnancy
During pregnancy, mild thrombocytopenia is comparatively common and usually has no implications either for mom or fetus. Although in most patients, there is no danger, thrombocytopenia may be a consequence of a variety of pathologies requiring closer surveillance and feasible treatment.
Read also: What is fetal growth reduction
For their prevalence and management problems, two clinical scenarios are particularly important. Firstly, isolated thrombocytopenia. Mainly, the differential diagnosis between main and gestational thrombocytopenia.
The second is pre-eclampsia-related thrombocytopenia. Mainly, with its appearance and difference from thrombotic thrombocytopenic purpura and hemolytic uremic syndrome.
What should you understand concerning thrombocytopenia in pregnancy?
If your number of platelets is only slightly below the average level, you or your baby shouldn’t have any issues, and no therapy is necessary. Your doctor or laboratory worker will continue to monitor your platelet count for the remainder of your pregnancy if it goes down. Once your child is born, your platelet concentrations will return to normal.
Physicians do not know why gestational thrombocytopenia occurs, but two variables can play a role.
Read also: Labor odd and weird signs
- Your body generates more fluid blood (plasma) during your pregnancy. It implies that the platelets are diluted and less per milliliter of blood. However, this does not influence how well the platelets function.
- Your body destroys platelets naturally if they are not used and substitutes new ones for them. This process accelerates during pregnancy. The outcome is that your blood platelets are fewer but younger and more prominent.
Read also: Facts about cinnamon abortion
Extra tests should be available if your platelet count drops below 100 million per ml of blood. It is classified as mild gestational thrombocytopenia by your physician. Severe thrombocytopenia is diagnosed with a blood count of less than 50 million per ml.
If you have severe or mild thrombocytopenia, you are more probable to develop a disease like lupus. It is when you attack healthy cells with your immune system.
Some of these moms seldom already have a thrombocytopenia form. It is called immune thrombocytopenic purpura (ITP), which is related to non-pregnancy. Symptoms of bruising and lilac, spontaneous bleeding, are triggered on the skin. Some medications, like heparin, may also influence your count of platelets.
What are the potential risks?
Below are some of the condition and treatment risks that you may encounter during your pregnancy stage:
1. Maternal hazards.
Maternal warnings of ITP steroid medication involve gestational diabetes, maternal hypertension, an increase in mass, osteoporosis, and psychoses. Large dosages of prednisolone could trigger early membrane damage, adrenal suppression, and a small boost in a fetal fissure in the first trimester.
The primary maternal problem at delivery is hemorrhage. Major obstetrical hemorrhage after vaginal delivery is rare even with severe thrombocytopenia. Platelets should be ready when they are delivered, but the timing of their application depends on the task progress and the end method of delivery.
2. Fetal risks.
ITP Gestational thrombocytopenia and ITP until after pregnancies may be hard to distinguish. Gestational thrombocytopenia for neonates is regarded to be entirely benign, while ITP can lead to the transplantation of antibodies into fetal/neonatal thrombocytopenia. The threat of neonatal thrombocytopenia and intracranial hemorrhage is the major problem for females with ITP. Platelet counts are less than 50x 109/L in about 10% of neonates with ITP mothers, and 5% of platelets with ITP counts less than 20x 109/L.
Read also: A womans body after a miscarriage
The correlation between maternal and neonatal platelets is weak, but some trials have shown that with lower maternal platelet counts, the relative risk of neonatal thrombocytopenia rises. The maternal therapy reaction does not automatically safeguard the neonate against thrombocytopenia growth.
A neonatal platelet number should be acquired at delivery, and vitamin K injection should be postponed until the platelet number is identified. The number of neonatal plates is seldom less than 10x 109/L. Lastly, the majority of neonatal hemorrhagic events occur 24 to 48 hours after the delivery when the platelet number is lowest. If the platelet count is normal, repeat counts are not necessary. Transcranial ultrasound is suggested in neonates with low platelet counts.
3. TTP / HUS.
The risk of IUGR, prematureness, and fetal death for the fetus are essential because of comprehensive placental ischemia. To reduce danger, early plasma exchange may be useful. Some trials have shown a 67 percent live birth rate with effective therapy.
Read also:
- Falling While Pregnant Third Trimester
- Low Platelets In Pregnancy Is it Normal or Serious
- Surprising Facts about Facial Hair Growth During Pregnancy